Students identify real-world challenges in clinical settings
Honors biomedical engineering major Jenna Averill spent her winter session inside operating rooms and outpatient clinics, not as a patient, but as a problem spotter. Through the University of Delaware’s Clinical Immersion Program, or BMEG 350: Clinical Immersion for Engineers, she logged 100 hours at Rothman Orthopaedics observing spine surgeons and engaging directly with patients and practitioners. The goal? To identify real-world challenges in healthcare that future biomedical engineers might one day solve.
Rothman Orthopaedics has partnered with the Clinical Immersion Program for multiple years and for good reason. The program benefits both students and practitioners.
“It has been a joy to work with the students from the BMEG Clinical Immersion Program,” said Dr. Alexander Vaccaro, president of Rothman Orthopaedic Institute. “They are extremely motivated, curious, and highly interactive with our staff. Their enthusiasm adds energy to our teaching. It’s refreshing to work with learners so invested in the process of discovery.”
“We have been participating for almost 10 years,” added Dr. Alan Hilibrand, the Joseph and Marie Field Professor of Spinal Surgery. “Each year we learn and benefit from the original thinking of these students who consistently bring forward new ideas for better ways to run our operating rooms and clinics.”
The partnership isn’t just about mentorship. It also provides surgeons and clinical staff a direct line to the next generation of biomedical innovators. Students like Jenna are trained to spot gaps that may be overlooked in a busy practice.
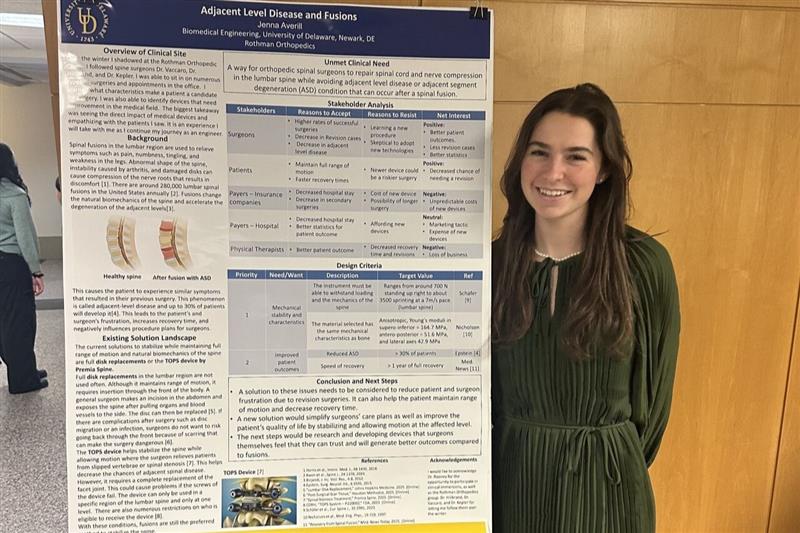
Jenna’s poster presentation at the Unmet Clinical Needs Poster Session on January 31 marked the end of her official immersion but not the end of her journey. She’s already thinking ahead to senior design and future internships, and hopes to work on solutions inspired by her time in the OR. Learn more about her experience below.
Q: What is the Clinical Immersion Program?
Jenna: It’s a 100-hour winter session program designed for biomedical engineering students to observe real clinical settings and identify unmet medical needs. It’s not mandatory, but it’s one of the most hands-on, eye-opening opportunities available in the major. The program really bridges what we learn in class with what’s happening in hospitals and clinics.
Q: Where were you placed, and what did you observe?
Jenna: I was incredibly fortunate to be placed at Rothman Orthopaedics, where I shadowed spine surgeons Dr. Alexander Vaccaro, Dr. Alan Hilibrand, and Dr. Christopher Kepler. I got to observe operating room procedures and outpatient clinic visits everything from diagnoses and pre-op consults to post-op care. It was inspiring to watch the level of coordination and trust between the entire medical team.
Q: Was there a particular moment during your time in the clinic that really stuck with you or shaped the way you think about biomedical engineering?
Jenna: Moments that stuck out to me were clinical visits where I was able to sit in with the patient and surgeon. I was able to listen to pre-op complaints and post-op check-ups. Hearing how life-changing the surgery was for the patient and how the surgeons helped give them their lives back was incredibly moving.
I was also fascinated by the surgeon’s process of creating treatment plans. It was compelling to see the connection between imaging and symptoms. You gain a whole new respect for healthcare providers when you see what goes on from their perspective. Dr. Hilibrand, Dr. Kepler, and Dr. Vaccaro are all so knowledgeable and determined it’s clear why they’re such outstanding surgeons.
The fellows Alex, Hunter, and Zach were also a huge part of my experience. They were kind, helpful, and always willing to answer my questions. Gaining that firsthand understanding of clinical processes and challenges gave me a completely new perspective on engineering problem-solving. I now better understand the specific criteria surgeons look for in solutions.
Q: What kind of project did you develop based on what you saw?
Jenna: Throughout the immersion, I documented over 20 potential unmet needs in spinal surgery. For the final poster session, I chose to focus on adjacent-level disease due to spinal fusion, a complication that occurs when a fusion surgery puts added stress on the vertebrae above or below the fused section. It’s common, but there’s still a lot of room for improvement in how we predict and prevent it. The experience showed me how crucial device design is in reducing long-term complications.
Q: What skills did you take away from this experience?
Jenna: I learned how to think more critically about medical device function and failure, ask focused questions in clinical environments, and communicate effectively with professionals outside my discipline. I also became more confident navigating the high-pressure atmosphere of an OR. These are skills I hope to carry into a career in medical device design or R&D, anywhere I can help develop tools that directly improve patient outcomes.
Q: How do you see this experience influencing your future, whether it’s in your classes, internships, or career path?
Jenna: This course has been the most valuable one I’ve taken as an undergraduate. It gave me the opportunity to build compassion by seeing the patient’s perspective, and it also helped me understand how medical products are actually used by providers.
Having clinical knowledge makes us better engineers. We develop a sharper sense of which solutions are truly feasible in a clinical setting. It also helps us form stronger working relationships with healthcare professionals, which is essential for collaborative problem-solving.
Dr. Vaccaro, Dr. Hilibrand, and Dr. Kepler all offered great advice for my future path. I think this experience has set me apart from my peers and also helped me figure out what I want to do. It reaffirmed my desire to be in the medical field, identifying problems and designing better solutions.