UD engineers are studying how robotic devices can guide personalized rehabilitation strategies for stroke patients
Every year in the United States, nearly 800,000 people have a stroke, and stroke survivors often experience reduced mobility and increased risk of long-term disabilities. The process of recovery and rehabilitation in this group of patients is both physically and mentally challenging and can take weeks or years before strength, control and sensation are fully regained.
Now, a team of researchers from the University of Delaware’s College of Engineering will be working towards improving post-stroke rehabilitation. With $1.2 million in funding from the National Institutes of Health, this project will use robotic exoskeleton devices and advanced modeling techniques to develop patient-specific exercises and interventions using a “therapeutic engineering” approach.
This work will be led by Panagiotis Artemiadis, an associate professor with joint appointments in the Departments of Mechanical Engineering and Biomedical Engineering. Collaborators and co-investigators, also with those joint appointments, are Fabrizio Sergi, an associate professor, Jill Higginson, professor and associate dean for Graduate and Post Graduate Education and director of the Institute for Engineering Driven Health, and Tom Buchanan, the George W. Laird Professor of Mechanical Engineering.
Post-stroke rehabilitation research
Previous and ongoing research projects at UD have focused on several aspects of the post-stroke rehabilitation process, from how the body perceives its location and movements (proprioception) to recovering a loss of language and speech abilities (aphasia).
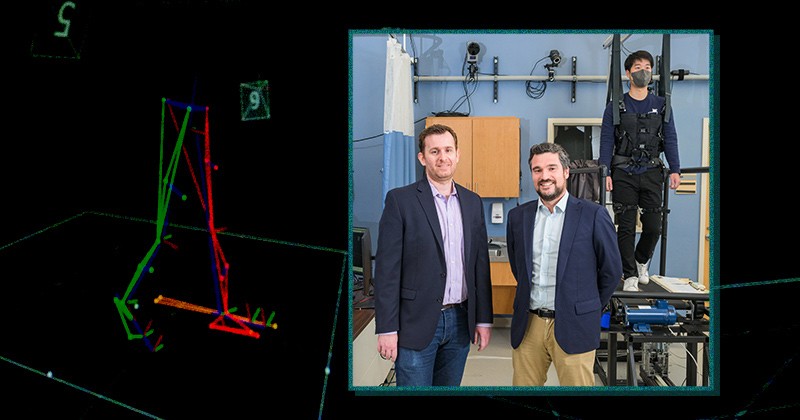
Doctoral student GilHwan Kim (right) demonstrates the robotic device and adaptive treadmill set-up, a unique approach that more closely mimics how patients will respond in real-world settings.
This newly-funded project led by Artemiadis builds off previous research on exoskeletons, work that was conducted as part of an NIH-funded project involving Buchanan, Higginson and Sunil Agrawal (now at Columbia University), and incorporates “a whole different approach and set of tools” towards improving post-stroke rehabilitation, said Buchanan.
“In some ways it’s continuing a theme that we started many, many years ago, but it’s using a whole new toolkit, and that’s what makes this really exciting,” Buchanan added.
Higginson said that the work also builds off her and Sergi’s research program through the GOALL project, which includes a focus on smaller “nudges” in movement with the help of robotic systems and adaptive treadmills. “Since then, Panos arrived on campus, and he brings a totally different flair that takes this work a step beyond,” Higginson said. “Overall, this new project is a really innovative way of looking at manipulating how someone’s moving.”
Precision and personalization
One of the main objectives of this research is to develop mathematical models of human gait and how the brain controls the motion of legs during walking, said Artemiadis. These models will be developed from data collected on a unique device, a variable-stiffness treadmill, which also allows for a more dynamic evaluation of a patient’s gait. The variable stiffness treadmill has been developed in Artemiadis’ lab and is used in various projects with humans and robot walkers.
“Once we have a representative model, a patient who needs gait rehabilitation could come to the clinic, and after evaluating specific things, such as joints, which muscles need to be re-activated, a personalized type of therapy can be proposed” said Artemiadis. “Our goal is to have a model for the individual that allows us to tailor exactly what the robot will do during therapy that can lead to better outcomes.”
Sergi said that one key advantage of this study’s design is the ability of the robotic device to deliver very precise interventions that help patients do the specific, repetitive motions that patients need to perform during the rehabilitation process.

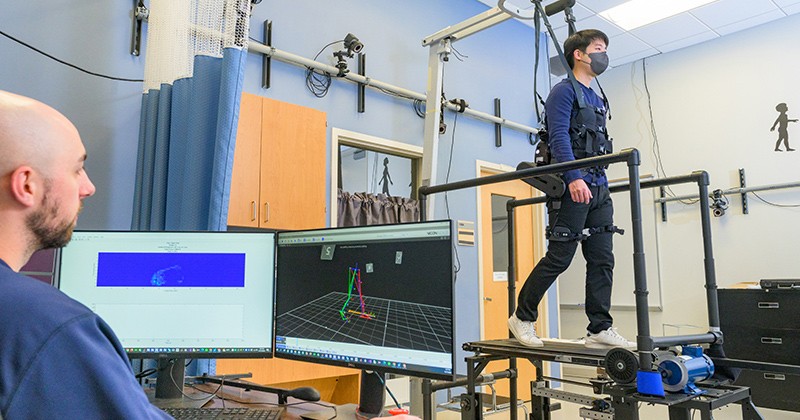
Doctoral student GilHwan Kim (right) using the adaptive treadmill device at the Human Robotics lab on UD’s Science, Technology and Advanced Research (STAR) Campus.
“In the context of walking, it’s important to provide mechanical stimuli in a way that is synchronized to the moment where it produces maximum propulsion. If you apply a force in a window of 150 milliseconds (ms), for example, you can use the model to ask what would happen if you applied that force 200 ms later,” said Sergi. “But in order to do that, you need to collect data that are in sync precisely with human walking, and you can only do that with an automatic system.”
“When you have a stroke, the connections between the brain and nerve cells die in a specific area, and only by practicing specific motions that you lost will make those connections again,” added Artemiadis. “The more that you practice the specific motions, the more the limb and the brain can relearn to control this motion. That’s why robot-assisted gait rehabilitation is so promising.”
And relying on an adaptive treadmill, which simulates how patients move outside of the clinic, could also improve retention, or how well patients are able to take what they’ve done in therapy and apply it in their day-to-day lives, said Higginson. “Being able to see those changes in real time, having the user experience that and learn what it feels like to walk at the faster speed because of the help that they’ve received can be beneficial,” she said.
Pushing the field forward
The researchers involved in this project will bring together a unique range of expertise towards addressing this research challenge — with Artemiadis’ knowledge of human-robot interactions, interlimb coordination and the study of gait in dynamic environments, Sergi’s research on wearable exoskeletons and propulsion during walking, and Higginson and Buchanan’s expertise in anatomy, biomechanics and neuromuscular control.

Jill Higginson (left), professor and associate dean for Graduate and Post Graduate Education and director of the Institute for Engineering Driven Health, and Tom Buchanan, the George W. Laird Professor of Mechanical Engineering, are also co-investigators on this grant.
“This project is a novel use of robotics applied to studying human walking, but the real strength of this work is the team that we have and the diversity in ways that different faculty members look at this problem,” said Buchanan. “It’s really exciting to be a part of this project.”
Along with improving the mobility of post-stroke patients, this work can also help researchers better understand human gait, which is crucial for developing more accurate models and new applications for robotics in healthcare, said Artemiadis.
“For robotic-assisted interventions, we need to know exactly what to do in order to involve the brain in this motion — it’s not just driving your legs to walk, it’s interacting with the legs and having a forceful interaction with the legs that makes this more efficient in terms of rehabilitation,” said Artemiadis.
One of the biggest challenges, for both the field as well as in this particular project, is to come up with a personalized treatment model, a challenge that is “also its main benefit,” said Sergi. “One of the main needs of this population is to improve mobility and walking, and these methods go in the direction of understanding how much we can customize therapeutic programs and movement-based therapies that are a part of stroke rehabilitation.”
Higginson said it’s fun to be part of a team that’s bringing together different areas of expertise.
“I’m looking forward to being able to apply the computational outcomes, based on all the experimental data, and being able to identify differences between interventions,” Higginson said. “I think that can be helpful to push the field forward.”
| Photos by Evan Krape | December 19, 2022